The Opaque Industry Secretly Inflating Prices for Prescription Drugs
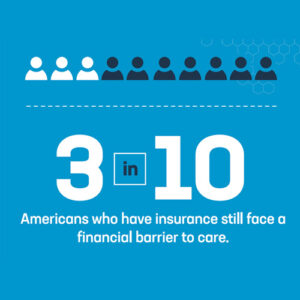
Americans are paying too much for prescription drugs. It is a common, longstanding complaint. And the culprits seem obvious: Drug companies. Insurers. A dysfunctional federal government.