
SC Pharmacy Association in support of H.3934
May 5, 2025 Dear Chairman Gagnon, I am writing to express our support for H. 3934, which will have a direct positive impact on the

May 5, 2025 Dear Chairman Gagnon, I am writing to express our support for H. 3934, which will have a direct positive impact on the

South Carolina gets an F because Ambetter from Absolute Total Care, BlueCross BlueShield of South Carolina, Molina Healthcare, InStil Health, and United Healthcare have copay
People living with serious, complex chronic illness such as HIV and viral hepatitis often rely on high-cost medications to manage their conditions and maintain their

In South Carolina, 400,000 adults 19-64 have no health insurance. 79% of SC small businesses – more than any state except Alaska – don’t offer
THE PROBLEMAs of July 2024, South Carolina remains one of 10 states that has yet to expand Medicaid coverage. That leaves almost half a million

Americans are paying too much for prescription drugs. It is a common, longstanding complaint. And the culprits seem obvious: Drug companies. Insurers. A dysfunctional federal government.

National Organization for Rare Disorders Mission StatementWe improve the health and well-being of people with rare disease by driving advances in care, research and policy.

United Healthcare and Prisma Health remain at the negotiation table two months after failing to reach an agreement over a price increase, leaving 58,000 South Carolinian patients disconnected from their healthcare providers.

Tiara Green, Interim CEO of Accessia Health March 17, 2024 Access to equitable, quality healthcare is a familiar and longstanding struggle for many U.S. families

Are you or someone you care about living with a rare disease? South Carolina’s Rare Disease Advisory Council (RDAC) welcomes your feedback on experiences navigating the disease.

By James Romano, BDASC Legislative Coordinator On a crisp January morning, the Bleeding Disorders Association of South Carolina (BDASC) hosted its second annual legislative breakfast.

WASHINGTON, DC – January 17, 2024 — Patient and provider groups were thrilled to learn
the US Department of Health and Human Services (HHS) dropped its appeal this week
challenging a US District Court ruling to make access to prescription drugs easier for people
living with serious, chronic conditions. This move ensures that the 2020 rule on cost-sharing is
in full effect, requiring insurers to count copay assistance towards patient cost-sharing. We now
urge HHS to enforce this ruling and issue immediate instructions to issuers on how to comply.
Historically Black Colleges and Universities (HBCUs) could soon become even bigger innovation hubs, thanks to measures advanced by Senator Raphael Warnock (D-Ga.). He recently introduced a bill to ensure that land-grant HBCUs receive fair funding, and last year, he fought to fund these institutions in the CHIPS and Science Act.
Greenville News: Your TurnSue Martin and Rhonda YoungGuest columnists Some South Carolina patients are being forced to choose between affording health care or putting food
Patients in South Carolina often rely on copay assistance to afford their medications. However, health insurers and pharmacy benefit managers (PBMs) are using the assistance

In a major victory for patients who depend on prescription drugs, Judge John D. Bates of the U.S. District Court for the District of Columbia struck down a Trump administration federal rule that allowed health insurers to not count drug manufacturer copay assistance towards a beneficiary’s out-of-pocket costs.
More than 105,000 people have in South Carolina lost healthcare coverage since June due to the state’s unwinding of the COVID-19 continuous Medicaid coverage protections. Unfortunately, 93% of individuals who lost coverage did so for procedural or paperwork reasons, not because individuals are no longer eligible. Because quality and affordable healthcare is critical to the 693,000 South Carolina residents living with lung disease, the American Lung Association is calling on Governor Henry McMaster to pause Medicaid redeterminations to improve its process so fewer people lose access to healthcare.
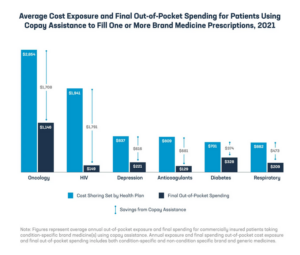
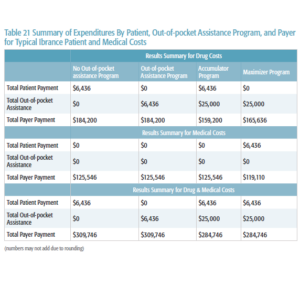
Health plans are increasingly using deductibles and coinsurance to shift more of the cost of care to chronically ill patients taking brand medicines. As data

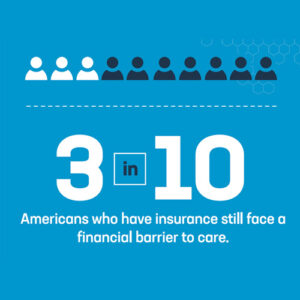
Too many Americans are struggling to access and afford their health care. While policy debates about how to address these issues can seem never ending,

With Congress discussing policy changes that would lower drug costs for patients and rein in powerful middlemen, insurers and their PBMs are dusting off their

The Global Healthy Living Foundation (GHLF) today refreshed a free, interactive tool showing that state laws banning accumulator and maximizer clauses in health insurance policies have not increased the cost of health insurance. In nineteen states, to date, these laws protect patient assistance programs (PAPs) by requiring that the financial assistance given to patients count toward their co-pays, deductibles, and out-of-pocket (OOP) maximums.
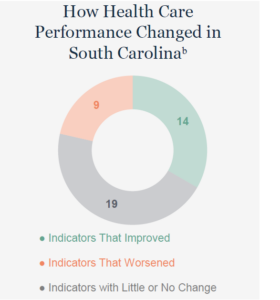
South Carolina ranks 37th in the U.S. in overall healthcare performance and among the bottom tier in several key metrics, a new nationwide scorecard shows. The Commonwealth Fund, a nonpartisan healthcare foundation, released its annual scorecard on Thursday. The scorecard reviewed all 50 states and the District of Columbia on 58 indicators, from reproductive and women’s health and access and affordability, to prevention and income disparity.

Understanding how health insurance works involves exploring how people feel about their
health coverage, how a!ordable that coverage is, how they interact with their insurance
provider, the problems they experience, and, critically, how insurance works for people when
they get sick. To accomplish this, the KFF Survey of Consumer Experiences with Health
Insurance interviewed a nationally representative sample of 3,605 U.S. adults with health insurance.

We Work for Health and Vital Transformation released a new study estimating that there would be 237 fewer FDA approvals of new medicines for patients battling cancer, neurological, and rare and infectious diseases (among others) over the next decade, as well as up to 1.1 million lost jobs if proposals to expand government-mandated drug pricing policies are implemented. Among the proposals under consideration is allowing Medicare to set prices for specific drugs five years after FDA approval, which would lead to devastating consequences for the biopharma ecosystem at an even more accelerated pace. These proposals are included in the White House’s FY 2024 budget as well as the Senate’s SMART Prices Act.

During BDASC’s 50th Anniversary Celebration Gala, BDASC was proud to present the Legislative Advocate of the Year Award to Representative Stewart Jones. Representative Jones has be instrumental in moving our bill into a bipartisan standing, by being the first republican to co-sponsor H.3618.

Since 2013, health insurance companies and pharmacy benefit managers (PBMs) have shifted the cost of medicines to patients by increasing the use of deductibles and coinsurance. In 2021, not only did 2 out of every 3 commercially insured patients taking brand name medications fill a prescription in the deductible phase or with coinsurance, but patients who paid in the deductible phase faced costs that were on average nearly 8 times higher than patients who filled prescriptions with copays.
COLUMBIA, S.C. After nationwide reports of texts and calls seeking money to obtain or keep Medicaid coverage, the South Carolina Department of Health and Human Services is warning the community about current Medicaid renewal scams that may target Healthy Connections Medicaid members.

COLUMBIA, S.C. – The South Carolina Department of Health and Human Services (SCDHHS) announced it will resume its standard Medicaid annual eligibility reviews April 1, 2023, to comply with provisions of the Consolidated Appropriations Act, 2023. This date marks the return of the agency’s standard annual review process that was in place prior to the COVID-19 federal public health emergency (PHE).

In the past few years, FEHB Carriers have approached OPM asking to integrate copay maximizer or optimizer programs in their plan offerings. These programs require a deviation in the prescription drug benefit design to capture savings from manufacturer non-needs-based copay assistance. Under 5 U.S.C. 8902(d), each FEHB contract “shall include such maximums, limitations, exclusions, and other definitions of benefits as [OPM] considers, necessary or desirable.” OPM has declined offering these programs in the FEHB Program and will not entertain any proposals that manipulate the prescription drug benefit design, or incorporate copay maximizer or optimizer programs, or other similar programs to capture such savings.
PBMs are diverting billions of dollars intended for patients and using that money to offset their own drug costs as well as to reward shadowy companies who arrange for the confiscation of those funds. While many business practices in healthcare can shock the conscience when they are exposed, the accumulator and maximizer issues stand out, as one group of companies is quite literally pilfering billions from another group of companies that were intended to assist patients in managing their out-of-pocket (OOP) costs.
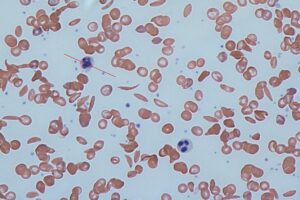
Sickle cell disease (SCD) is a genetic disorder that affects millions of people worldwide. The disease is caused by a mutation in the hemoglobin gene, which leads to the formation of abnormal hemoglobin molecules. These molecules can cause red blood cells to become stiff and sickle-shaped, leading to a range of health complications.

In the latest edition of NORD’s State Report Card we analyze all 50 states and Washington, D.C., on nine policy issues that impact the rare disease community. Each state has their own individual report card.

Health care disparities create undue and significant hurdles for patients in need and disproportionately impact individuals with chronic conditions. It is critical that all patients have equal access to health care services independent of age, ethnicity, socio-economic status or health status.

The cost of health care is increasing at an exponential rate. Patients with chronic illnesses who are already struggling to make ends meet simply cannot afford the cost of their medical treatment. This is troubling news for a state where 60% of the adult population is living with a chronic illness. Hitting even closer to home, the South Carolina Department of Health and Environmental Control reported Clarendon as one of the counties in our state with the highest rate of individuals suffering with two or more chronic illnesses.

Patients with rare, complex, or chronic diseases such as HIV and viral hepatitis often need high-cost medications to manage their conditions and maintain their health. For many of these medications, there is no generic or less expensive alternative.

Important changes are coming to Healthy Connections Medicaid. Do you or a family member currently have health coverage through Medicaid or the Children’s Health Insurance Program (CHIP)? If so, you may soon need to take steps to find out if you can continue your coverage.

Faced with high costs at the pharmacy counter, a growing share of commercially insured patients rely on copay assistance programs offered by pharmaceutical manufacturers to help them pay their out-of-pocket costs.

We all know someone who has struggled with the cost of health care. In many cases, particularly with chronic illnesses, the costs become so expensive, many patients find themselves having to make the difficult decision of whether to pay for food or gas or their medicine.

When a stubborn pain in Nick van Terheyden’s bones would not subside, his doctor had a hunch what was wrong. Without enough vitamin D in the blood, the body will pull that vital nutrient from the bones. Left untreated, a vitamin D deficiency can lead to osteoporosis. A blood test in the fall of 2021 confirmed the doctor’s diagnosis, and van Terheyden expected his company’s insurance plan, managed by Cigna, to cover the cost of the bloodwork. Instead, Cigna sent van Terheyden a letter explaining that it would not pay for the $350 test because it was not “medically necessary.”
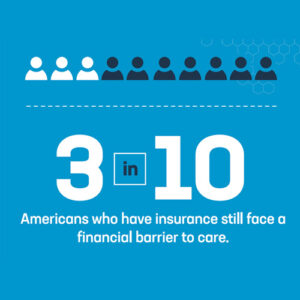
Patients continue to show up at the pharmacy counter and realize their commercial health insurance coverage doesn’t provide the level of access and affordability they need.