 STATUS INFORMATION
STATUS INFORMATION
General Bill
Sponsor: Representative Henegan
Introduced in the House on January 11, 2023
Currently residing in the House:
Referred to Committee on Labor, Commerce, and Industry
Summary: Pharmacy Benefits
A BILL TO AMEND THE SOUTH CAROLINA CODE OF LAWS BY ADDING SECTIONS 38-71-292 AND 38-71-820 BOTH SO AS TO DEFINE TERMS AND OUTLINE THE APPLICABILITY AND REQUIREMENTS FOR COST SHARING FOR INSURERS; BY ADDING SECTION 38-71-2270 SO AS TO DEFINE TERMS AND OUTLINE THE APPLICABILITY AND REQUIREMENTS FOR COST SHARING FOR PHARMACY BENEFIT MANAGERS; AND BY AMENDING SECTION 38-71-2200, RELATING TO DEFINITIONS, SO AS TO MAKE CONFORMING CHANGES.
1/11/23 House Introduced and read first time (House Journal-page 40)
1/11/23 House Referred to Committee on Labor, Commerce and Industry (House Journal-page 40)
Bill Sponsors: (updated 5/28/24)
REPUBLICAN
Rep. Stewart Jones (R-14)
Rep. Richie Yow (R-53)
Rep. Cody Mitchell (R-65)
Rep. Tommy Pope (R-47)
Rep. David Vaughan (R-27)
Rep. Anne Thayer (R-9)
Rep. Jerry Carter (R-3)
Rep. Max Hyde (R-32)
Rep. Val Guest (R-106
Rep. Brandon Newton (R-45)
Rep. Heather Crawford (R-68)
Rep. Tim McGinnis (R-56)
Rep. Kevin Hardee (R-105)
Rep. Case Brittain (R-107)
Rep. William Bailey (R-104)
Rep. Don Chapman (R-8)
Rep. Carla Schuessler (R-61)
Rep. April Cromer (R-6)
Rep. Mike Burns (R-17)
Rep. Craig Gagnon (R-11)
Rep. Bill Hixon (R-83)
Rep. Bill Taylor (R-86)
Rep. Joe White (R-40)
Rep. Jason Elliott (R-22)
Rep. Sylleste Davis (R-100)
Rep. Brandon Cox (R-92)
Rep. Tom Hartnett (R-110)
Rep. Marvin Smith (R-99)
Rep. Jay Kilmartin (R-85)
Rep. Jeff Johnson (R-58)
Rep. Jordan Pace (R-117)
Rep. Mike Neese (R-44)
Rep. Robby Robbins (R-97)
Rep. Brian Lawson (R-30)
Rep. Brandon Guffey (R-48)
Rep. Gary Brewer (R-114)
Rep. Lee Hewitt (R-108)
Rep. Bill Herbkersman (R-118)
Rep. Neal. Collins (R- 5)
DEMOCRAT
Rep. Pat Henegan (D-51)
Rep. Robert Williams (D-62)
Rep. Ivory Thigpen (D-79)
Rep. John King (D-49)
Rep. Wendell Jones (D-25)
Rep. Rosalyn Henderson-Myers (D-31)
Rep. Roger Kirby (D-101)
Rep. Chandra Dillard (D-23)
Rep. Annie McDaniel (D-41)
Rep. Jermaine Johnson (D-70)
Rep. Beth Bernstein (D-78)
Rep. Heather Bauer (D-75)
Rep. Gilda Cobb-Hunter (D-95)
Rep. Spencer Wetmore (D-115)
Rep. Will Wheeler (D-50)
Rep. Joseph Jefferson (D-102)
Rep. Lucas Atkinson (D-57)
Rep. Wendell Gilliard (D-111)
Rep. Michael Rivers (D-121)
Rep. Jackie “Coach” Hayes (D-55)
Rep. JA Moore (D-15)
Rep. Kambrell Garvin (D-77)
Rep. Carl Anderson (D-103)
Rep. Leon Stavrinakis (D-119)
The Problem
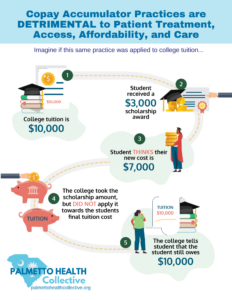
In the commercial health insurance market, some patients are being forced to pay more out-of-pocket for their medicines due to an increase in deductibles and the use of coinsurance instead of copays. Deductibles require patients to pay in full for their medicines before insurance coverage kicks in. And unlike copays, which are a fixed dollar amount charged per prescription, coinsurance requires patients to pay a percentage of the medicine’s price.
The Solution – Make All Copays Count
To help patients better access their medicine and stay adherent, many third-party entities, including pharmaceutical manufacturers, offer cost-sharing assistance. Historically, commercial health insurance plans counted this assistance towards a patient’s deductible and maximum out-of-pocket, providing relief from high-cost sharing and making it easier for patients to get their medicines.
South Carolina should enact a law to protect patients who rely on third-party cost-sharing assistance by ensuring that all payments – made by the patient or on behalf of the patient – count towards the patient’s deductible and out-of-pocket maximum. Sixteen states, including neighboring Georgia, North Carolina, and Virginia, have already enacted legislation to address this issue.
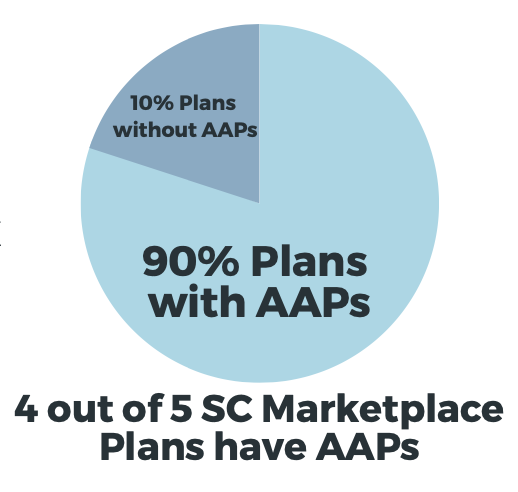
Unfortunately, health insurers and PBMs have adopted Polices, often referred to as “accumulator adjustment programs” that block assistance towards a patient’s deductible and maximum out-of- pocket limits CoPay Assistance.
The following groups have committed to advocate on behalf of SC H.3618
- Aimed Alliance
- aHUS Action Network
- ALS Association
- American Diabetes Association
- American Cancer Society Cancer Action Network
- Association for Clinical Oncology (ASCO)
- Arthritis Foundation
- Bleeding Disorders Association of South Carolina
- Coalition of State Rheumatology Organizations
- Community Oncology Alliance (COA)
- Everylife Foundation of Rare Diseases
- Gaucher Community Alliance
- Hemophilia Federation of America
- International Foundation for AiArthritis
- Lupus and Allied Diseases Association, INC
- Multiple Sclerosis Association of America
- National Alliance on Mental Illness, SC
- National Eczema Association
- National Bleeding Disorders Foundation
- National Psoriasis Foundation
- SC Oncology Society (SCOC)
- South Carolina Advocates for Epilepsy
- Spondylitis Association of America
- wAIHA Warriors
Additional Resources
Members of the Bleeding Disorders Association of South Carolina gathered for training on Rare Disease Day in preparation for their Annual State Awareness and Legislative Day held on March 1st at the State Capitol in Columbia. The 2023 priorities were advocating for passing H.3618 and continued funding for the state Hemophilia Assistance Program.
Members of the Bleeding Disorders Association of South Carolina gathered to celebrate the chapter’s 50th Anniversary. During this celebration, the chapter awarded Representative Stewart Jones with their Legislative Advocate of the Year award. Representative Jones received this award for his support of House Bill 3618. With his support, H.3618 became a bipartisan bill.